15. The Right Way to Evaluate a Concussion
/The Trip Begins
Last week I outlined how things work at the Sports Neurology Clinic in Michigan, and this week I want to write about my experience during my first visit there. Before heading to the clinic in May, I received a schedule of the various appointments I was to attend. First on the list was an appointment with Dr. Kutcher, the neurologist and founder of the Sports Neurology Clinic.
Dr. Kutcher has a domineering presence; he is well over six feet tall with light brown hair and a clean-cut beard. He gave me a firm handshake and comforting smile when we first met, as if assuring me through his stature that I was in good hands. This doctor knew what he was doing, I thought. He might be able to help me.
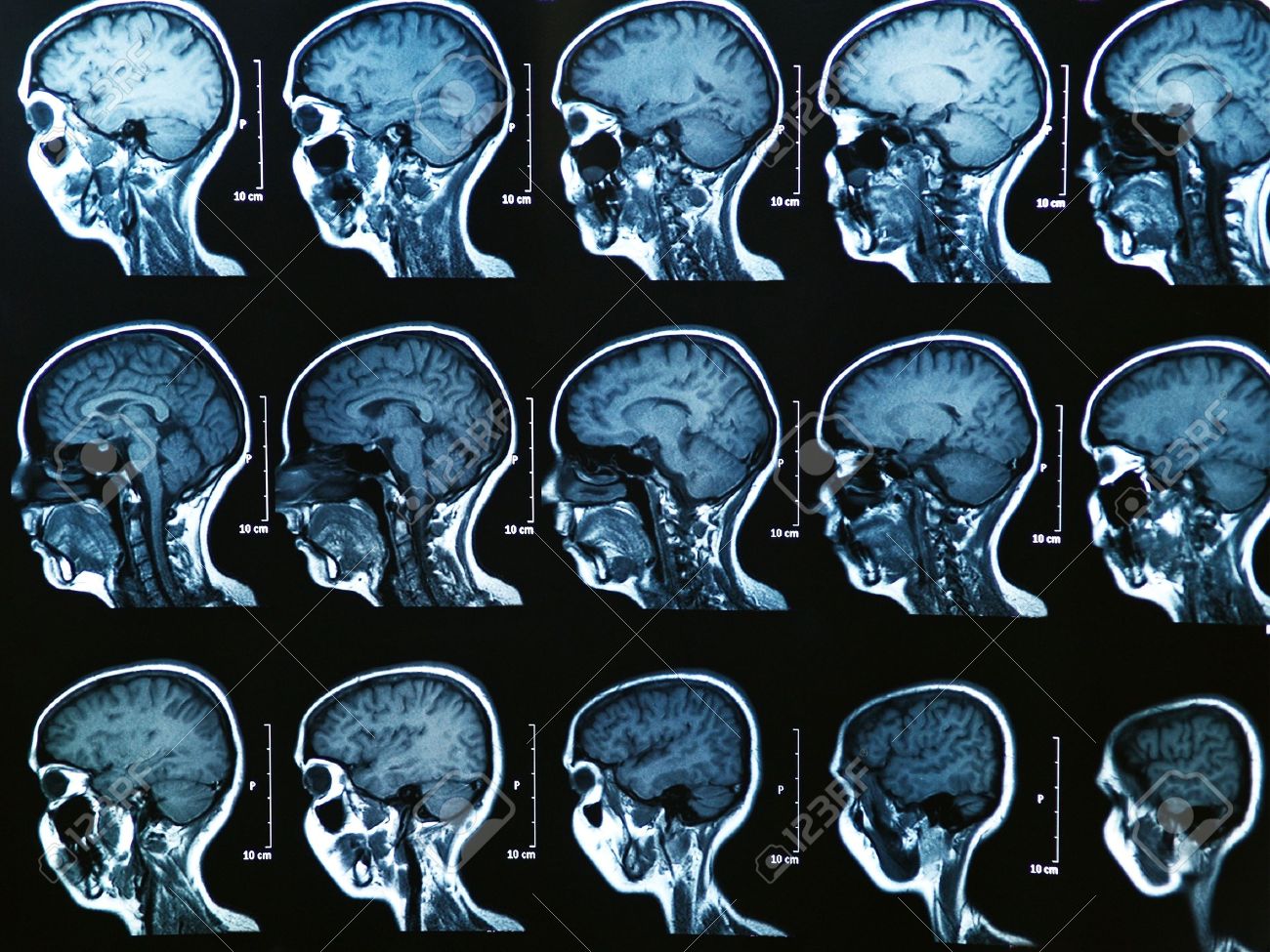
Dr. Kutcher wanted all of the details of my story; he was patient and listened intently, he asked pointed questions, he took notes on his computer, and occasionally chimed in to offer much needed expertise. He was the first doctor to actually take the time to open up the MRI’s of both my brain and neck and go over them with me.
Then he had me take a Brain Network Activity (BNA) test to monitor how my brain waves were changing while undergoing a series of tasks. This creates a temporal map of the neuron networks within the brain, which looks different in concussed individuals versus healthy individuals. Luckily, the BNA test revealed that the networks in my brain looked fine, supporting the theory that my concussion had healed and my symptoms were being driven by another issue, whether psychological, structural or something else.
However, before concluding what exactly was driving my symptoms, he needed to wait and hear the findings from the other doctors on my team. Our roughly three-hours together concluded with me asking a very simple question: “Do you think you can help me?”
Dr. Kutcher looked at me, took a deep breath and said, “It’s complex. But yes, I think that we can.”
The Neck Evaluation
The next day, I was scheduled for a workout with the clinic’s athletic trainer (something I was absolutely dreading), an evaluation by the vestibular doctor, and finally, an appointment with Dr. Colwell, the Physical Medicine and Rehabilitation doctor.
The workout went as expected; all of my symptoms significantly increased after twenty minutes on the bike with my heart rate around 120 beats per minute. Unfortunately for me, they didn’t just worsen for a few hours, but for several days after exertion of this nature. The vestibular evaluation also went as expected; there was nothing wrong with my eye movements, balance or coordination.
My appointment with Dr. Colwell, the doctor who would assess my neck, was later that afternoon. I knew he would be the doctor that would make or break it for me. If I had any chance at recovering, it would be because of him. I remember sitting in the waiting room with my mom, anxiously anticipating the nurse to call my name and lead me into an appointment room for yet another evaluation by yet another doctor.
I meticulously scanned my surroundings just as I had the day I traveled to Avon, where I received fourteen prolotherapy injections in my neck. The waiting room was large and crowded, bustling with administrators checking people in and out, doctors and nurses diligently moving about the halls while patients waited for their turn to be seen.
Could this be the place?
It couldn’t be, I thought. What’s the point in even being here? I wanted to get up and leave. My head hurt so much I cursed the fact that I had to sit waiting without anything to support my neck. I desperately wanted to return to the hotel and lay in bed, lights off, blinds shut. To my familiar, safe haven.
Yet before I had time to call it quits my name was called and I was shuttled into an appointment room down the hall. After a few standard questions by the nurse, Dr. Colwell himself soon walked in and greeted me. Like Dr. Kutcher, he was also quite tall. He bore a gentle, welcoming smile and had soft blue eyes that lay behind rectangular framed glasses.
Unlike so many other doctors visits throughout this experience, Dr. Colwell was very well prepared for our appointment. He had already looked through my file, including my health history and all four of my MRI’s, and he had read through a detailed email from Dr. Kutcher about my visit with him the day prior. His preparedness was refreshing, and I took it as a good sign of what was to come.
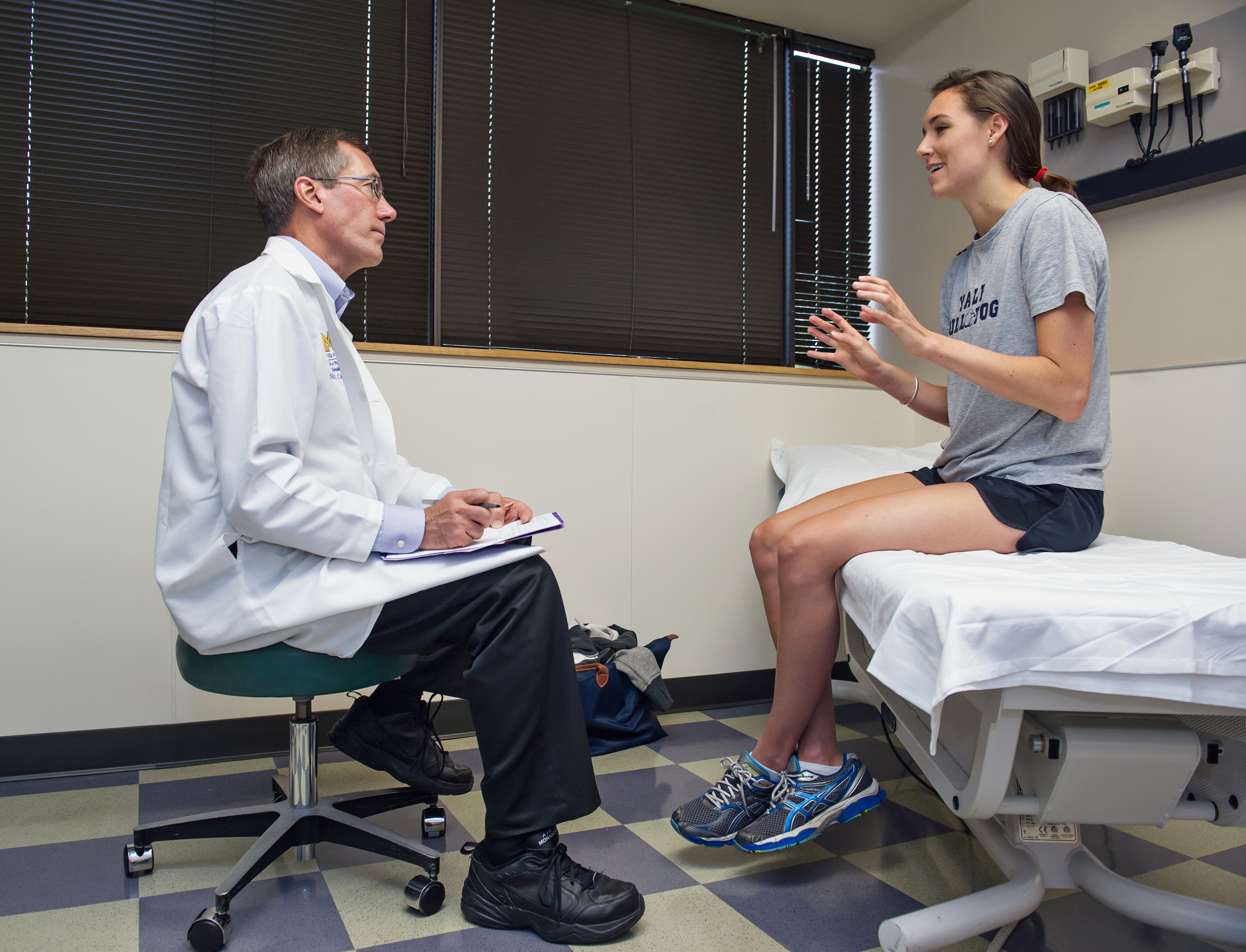
Dr. Colwell asked several questions about my injury, and I welcomed them freely. As I spoke I could tell he was thinking critically about my case, adding and detracting theories from what he would later call his “differential list”. This list detailed all the possible things that might be contributing to my problem, which was an approach that became one of the many things I love about Dr. Colwell. As we began to “peel back the layers of the onion”, another coined phrase that I love, he narrowed his differential list until a clear picture about my case was formed. It was a tactical, Type-A approach that I deeply appreciated.
Before making any concrete conclusions, however, Dr. Colwell walked me through a thorough physical exam. He didn’t just evaluate the restrictions and damage in my neck, he included my entire body as well. He identified a number of problems, the majority of which stemmed from the upper right portion of my neck. This was the same area that, when injected with prolotherapy in Vancouver, completely took away my headache. The fact that he identified this area as a major problem was another a good sign for me. It meant he knew what he was doing and that there were important issues to be addressed.
The black dot represents the location of the trigger point and the red dots are the corresponding pain locales.
He concluded that the restrictions in my neck and the subsequent pain I was experiencing in my head were consistent with Janet Travell’s Trigger Point Patterns. Travell was a physician who researched the concept of trigger points as the cause of musculoskeletal referred pain. These trigger points are hyperirritable, tender nodules in the muscles fascia, which can produce pain in broader, distant areas of the body. In my case, the trigger points and associated muscle tension in my neck were sending intense, referral pain into my head.
Dr. Colwell took the time to open an anatomy book and use visuals to explain this concept further. He also provided more detail on the areas of my neck that were damaged and how they contributed to my concussion symptoms, which I described in a previous post.
The Next Steps
From there, Dr. Colwell conferred with Dr. Kutcher and we all discussed my treatment plan moving forward. Dr. Colwell put together a detailed plan to address the structural damage he identified, and Dr. Kutcher advised that I slowly begin to re-introduce exercise into my life. Although at that point I didn’t feel comfortable or capable of doing any exercise, I agreed to give it a try once my symptoms started improving.
With all of this, I left Michigan with something very critical to my recovery – a concept I had completely lost sight of for many months – hope. I left feeling like maybe I wasn’t doomed after all. I couldn’t be certain because, quite frankly, I didn’t feel any better than when I arrived. But I was okay with that because now I had a recovery path. Now I had a plan to get well that I actually believed in, which is all I could ask for and all I had wanted since the very start of this journey.
And so began the next phase of my recovery, one I welcomed and was very eager to commence: rehab.



